Metabolic Health and Tendinopathy: Why Load Alone Does Not Explain Tendon Pain
- Luke Nelson

- 2 days ago
- 4 min read

When we think about tendinopathy, the usual explanation is simple:too much load, too soon, for too long.
And while training load absolutely matters, it is no longer enough to explain why:
Some people develop persistent tendon pain
Some struggle to improve despite “perfect” rehab
And some tendons fail at surprisingly low loads
Increasingly, research is pointing to something else playing a major role:
👉 metabolic health
Diabetes, obesity, and lipid disorders do not just affect the heart and blood vessels. They also change how tendons are built, how they adapt to load, and how well they heal.
Tendinopathy is not just a mechanical problem. It is a mechanical plus biological problem.
Tendons Adapt to Load, But Only If the Biology Allows It
Under normal conditions, tendon responds to loading by:
increasing collagen synthesis
improving stiffness and strength
maintaining organised fibre structure
This is the principle behind eccentric training, heavy slow resistance, and graded loading programs.
But tendon adaptation depends on a healthy cellular environment.
Metabolic disorders interfere with this process by:
altering collagen cross-linking
impairing blood supply
promoting low-grade inflammation
disrupting tendon stem cell function
As a result, tendons exposed to the same training load may respond very differently depending on the person’s metabolic status (Kuliś et al., 2025; De Luca et al., 2025).

Diabetes: One of the Strongest Risk Factors for Tendinopathy
Among all metabolic conditions, diabetes shows the most consistent association with tendon disease.
A large systematic review and meta-analysis found:
people with diabetes had around a 7-fold higher risk of Achilles tendinopathy
higher rates of trigger finger, medial epicondylitis, and shoulder tendinopathy
poorer healing and higher re-tear rates after tendon surgery
(De Luca et al., 2025; Abate et al., 2013)
Why?
Chronic hyperglycaemia leads to the formation of advanced glycation end-products (AGEs).These molecules:
Stiffen collagen fibres
Make tendon tissue more brittle
Impair cellular repair mechanisms
Histological studies show diabetic tendons have:
Disorganised collagen
Reduced elasticity
Poorer vascular supply
In simple terms, the tendon becomes structurally inferior before loading even begins.

Obesity Is Not Just About Body Weight
It is tempting to think obesity affects tendons simply because heavier bodies load tendons more.
But this is only part of the story.
Adipose tissue acts as an endocrine organ. In obesity, it releases:
TNF-α
IL-6
Leptin
Other inflammatory mediators
This creates a state of chronic low-grade systemic inflammation that directly affects tendon tissue (Lui and Yung, 2021).
This inflammatory environment promotes:
Collagen breakdown
Disorganised tendon matrix
Impaired healing
Persistent pain signalling
This explains why obesity is linked to:
Higher rates of Achilles and rotator cuff tendinopathy
Worse post-surgical outcomes
Higher recurrence rates
(Abate et al., 2013; Lai et al., 2024)
So obesity affects tendons through:
Mechanical overload
Inflammatory biology
Both matter.

Cholesterol and Lipids: The Overlooked Tendon Risk
Dyslipidaemia is another underappreciated contributor.
High cholesterol has been associated with:
Achilles tendon thickening
Xanthomas, which are lipid deposits within tendons
Collagen disorganisation
(Abate et al., 2013; De Luca et al., 2025)
Lipid disorders appear to:
Disrupt tendon stem cell activity
Alter collagen turnover
Reduce tensile strength
This is why:
Achilles tendinopathy is common in people with familial hypercholesterolaemia
Lipid abnormalities are frequently found in chronic tendinopathy populations
While statins remain controversial, the metabolic condition itself appears to carry intrinsic tendon risk.

Metabolic Syndrome: When Risks Stack
Metabolic syndrome combines:
Central obesity
Insulin resistance
Dyslipidaemia
Hypertension
It represents a perfect storm for tendon pathology.
Studies show that people with metabolic syndrome:
Have significantly higher rates of Achilles tendinopathy
Respond less favourably to traditional loading programs
Experience more persistent symptoms
(Kuliś et al., 2025; Lai et al., 2024)
This helps explain why some patients:
Follow rehab correctly
Progress load sensibly
But still plateau or relapse
The tendon is being loaded in a biologically hostile environment.

Why “Perfect” Rehab Sometimes Fails
Traditional rehab models assume:
apply load, tendon adapts, pain improves
But metabolic disease changes this equation.
Evidence suggests:
Eccentric and heavy loading programs are less effective in metabolically unhealthy patients
Collagen remodelling is slower
Flare-ups are more common
Adaptation thresholds are lower
(Kuliś et al., 2025)
This does not mean loading is wrong. It means loading alone may be insufficient.

Clinical Implications: What Should Change in Practice?
For clinicians, metabolic health should become part of tendon risk stratification, especially in:
Bilateral tendinopathy
Recurrent cases
Slow or incomplete rehab response
Atraumatic onset
Middle-aged and older runners
Key screening considerations:
HbA1c or known diabetes
Lipid profile
BMI and waist circumference
Features of metabolic syndrome
(De Luca et al., 2025)
Rehab still needs mechanical loading. But it should be paired with:
Education about metabolic contributors
Coordination with GP or physician where appropriate
Realistic timelines
Conservative progression strategies

What Runners Should Take From This
For runners, the message is not “don’t train”.
It is:
your tendons adapt based on both training and biology
Training matters. So does:
Sleep
Nutrition
Body composition stability
Blood sugar control
Lipid health
You can have an excellent training structure and still struggle if your metabolic health is working against your tendons.
Healthy metabolism improves:
Tissue quality
Recovery
Load tolerance
Long-term durability

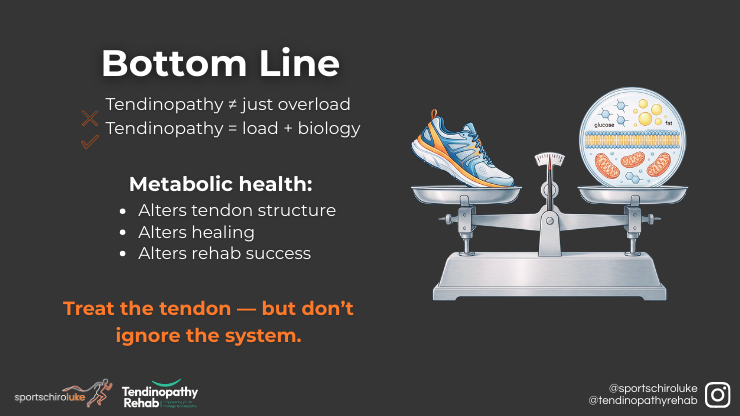
Bottom Line
Tendinopathy is not just about overload.
It reflects:
how much load you apply
and how capable the tendon is of adapting
Metabolic health influences:
tendon structure
healing capacity
rehab response
recurrence risk
Ignoring this leaves part of the problem untreated.
The future of tendon care is not:
load or biology
It is:
load plus biology
References
Abate, M., Schiavone, C., Salini, V. and Andia, I. (2013) ‘Occurrence of tendon pathologies in metabolic disorders’, Rheumatology, 52(4), pp. 599 to 608.
De Luca, P. et al. (2025) ‘The interplay between metabolic disorders and tendinopathies: systematic review and meta-analysis’, Journal of Experimental Orthopaedics, 12, e70429.
Kuliś, S. et al. (2025) ‘Beyond mechanical load: metabolic factors and advanced rehabilitation in sports tendinopathy’, Journal of Clinical Medicine, 14(21), 7480.
Lai, C. et al. (2024) ‘Metabolic syndrome and tendon disease: a comprehensive review’, Diabetes, Metabolic Syndrome and Obesity, 17, pp. 1597 to 1609.
Lui, P.P.Y. and Yung, P.S.H. (2021) ‘Inflammatory mechanisms linking obesity and tendinopathy’, Journal of Orthopaedic Translation, 31, pp. 80 to 90.



